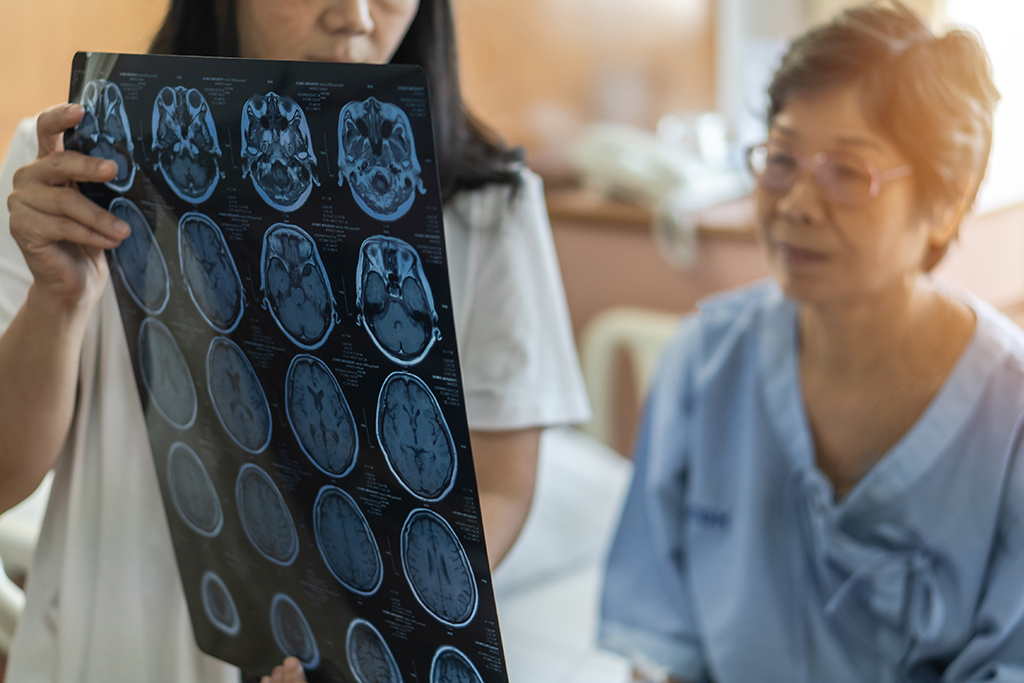
Physicians in Wilmington Health Neurology diagnose and treat disorders of the central and peripheral nervous systems, which include the brain, spinal cord, and nerves in the body. Patients who suffer from headaches, back and neck problems, seizures, memory loss, and other brain disorders may seek the assistance of a neurologist. Neurologists also diagnose and treat muscle diseases and diagnose or rule out conditions such as epilepsy, brain tumors, brain injuries, and stroke.
Wilmington Health’s state-of-the-art equipment enables us to perform testing and analysis on-site without referring patients out of the area.