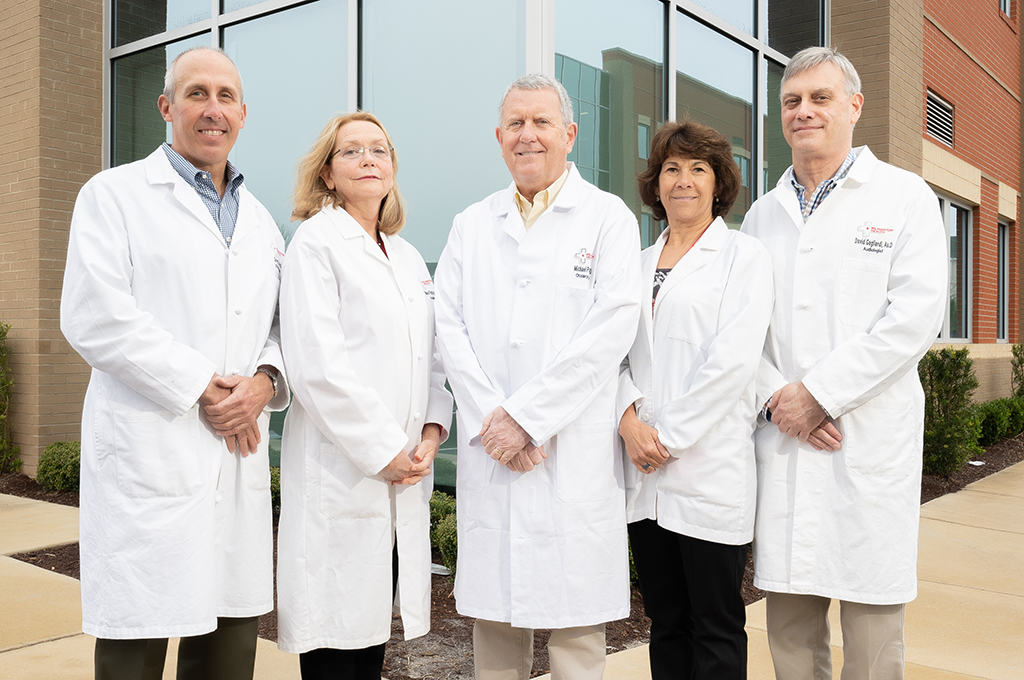
Wilmington Health otolaryngologists, commonly referred to as ENT physicians, are physicians certified in the medical and surgical management and treatment of diseases and disorders of the ear, nose, throat, and related structures of the head and neck. Our ENT team treats patients of all ages.
Our special skills include diagnosing and managing diseases of the ears, sinuses, voice box, mouth, throat, and structures in the neck and face of children and adults.