Wilmington Health believes that your community is our community. We are an industry leader in quality care, and our caregivers and staff extend compassion to those in need and help to improve the health and well-being of those we serve, by focusing on inclusive evidence-based medicine and creating long-term, sustained investments to prevent disease and promote health. We are a health system and services platform that continues to evolve in lockstep with community need. We want the same things that our patients want: healthier communities that lead to healthier tomorrows.
BECOMING A HIGH-PERFORMANCE HEALTH SYSTEM
Wilmington Health’s journey to becoming a High-Performance Health System (HPHS) began over a decade ago. We took a programmatic approach by implementing a three-part system of change. This included our leadership setting organizational direction to us becoming an HPHS; our robust process of monitoring, evaluating, and improving at the point of service delivery; and a redesign of the most elemental processes throughout the organization.
Today, our priority is understanding how our changes impact the total cost of care. With this priority, we pay careful attention to setting metrics, developing thought-provoking analysis, and critiquing each innovation to identify cost-saving opportunities. We continue to strive to give our patients quality care at a low cost by using cutting-edge technology and by also participating in the latest research.
Innovation and transformation have continued to be our backbone and have assisted us in achieving outstanding performance when ranked nationally among our peers and much larger health systems.
ENGAGING PATIENTS
Wilmington Health puts your experience first. We understand that your feedback and collaboration are the most important measures of the quality of care we provide.
To engage patients in their care and for them to let us know how we’re doing, we routinely survey our patients and share insights, feedback, and evaluations to our entire team of providers and staff. With each round of surveys, we collaborate with our division chiefs, leadership, and supporting staff on ways to improve patient engagement and satisfaction. We also publish patient satisfaction performance results to individual providers, which are available to anyone who visits a provider’s page on our web site.
Our most recent survey showed that patients rate our providers at or above the national average for every question asked.
HOW WE LOWER COSTS
We commit to providing our patients with consistent transparency on our cost and quality. Nationally, health care organizations and self-insured employers are focusing more on wellness and prevention, to divert from otherwise high-cost procedures and prognoses. Achieving market leadership in cost containment requires excelling at reimbursement competencies and risk-based capabilities. We constantly evaluate every process and procedure across our organization to eliminate fiscal waste. Additionally and most notably, our superlative analytic team proactively identifies our high-risk patients so we can deliver care at the right time in the best setting. We have stood up our Today’s Care Clinics, where we have staffed Emergency Room Physicians to avoid unnecessary and costly ER visits. We have also added patient resources such as our Chronic Care Management, ER Avoidance, and Diabetic Education Programs. Wilmington Health recognizes the best way to lower our costs in care is by transparently and consistently evaluating and implementing ways to support our patients.
IMPROVING QUALITY OF CARE
We continue to track national quality measures and compare our scores to providers across the country. Our state-of-the-art electronic health record system (EHR) allows us to compile and analyze data to see how we are doing as an organization; how our physicians are doing; and most importantly, how our patients are doing.
The EHR also lets us focus on population health: looking at how our providers are doing among populations of patients. We can identify high-risk patients, review clinical outcomes, and develop or partner with quality improvement programs to support our community. Wilmington Health is participating in the Medicare Direct Contracting Program, which is a risk-sharing program aimed at reducing expenditures and preserving or enhancing the quality of care for patients. We also participate in other quality arrangements with commercial and Medicare Advantage payers, such as Humana, Blue Cross Blue Shield, Aetna, and United Healthcare.
Check out our past quality and financial performance to see how much money Wilmington Health has saved the health care system and improved the quality of our patients’ care. www.physicianshealthcarecollaborative.com
What does this mean for Patients?
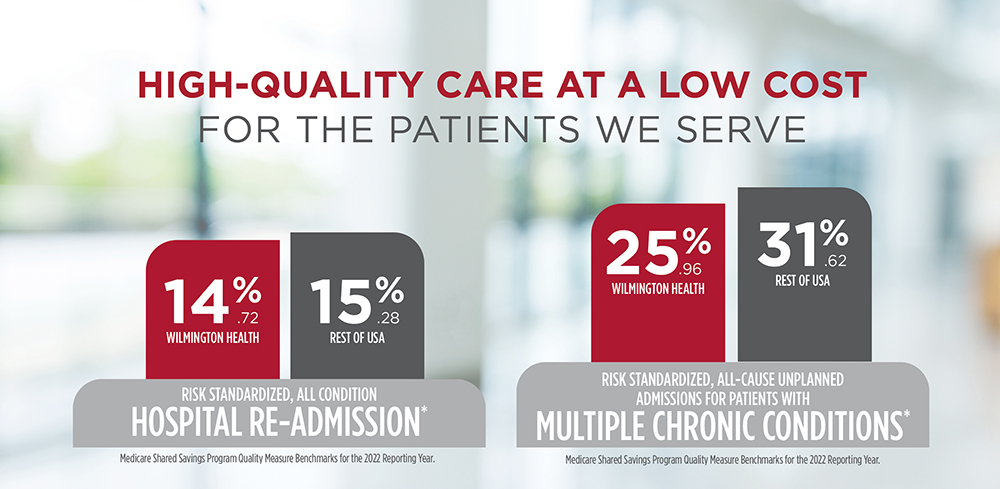
Emergency Department visits and hospital admissions are two costly services that can often be avoided. Through our Today’s Care locations, we provide your employees with alternatives to the ED. Additionally, by keeping our patients healthy we saved Medicare over 14 million dollars in 2022. This reduces the cost of care for your employees and costly claims on your health plan.
Breast Cancer Screening
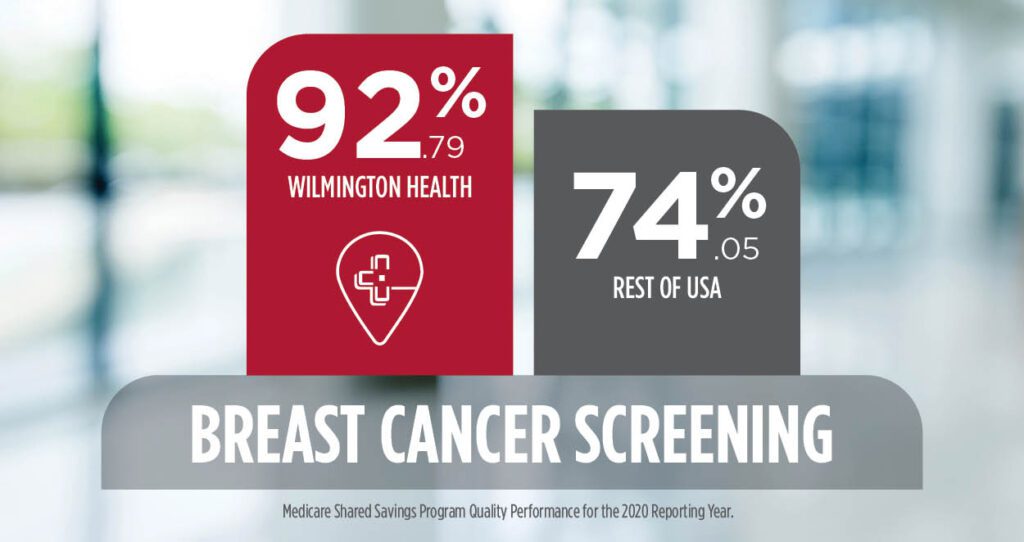
When it comes to breast cancer screenings, Wilmington Health is nearly 18% higher than all other providers in the United States! Breast cancer that’s found early is often easier to treat because it hasn’t spread beyond the breast. This improves the outlook for our patients and could save billions of dollars on breast cancer treatments.
Diabetes Mellitus: Hemoglobin A1C Poor Control
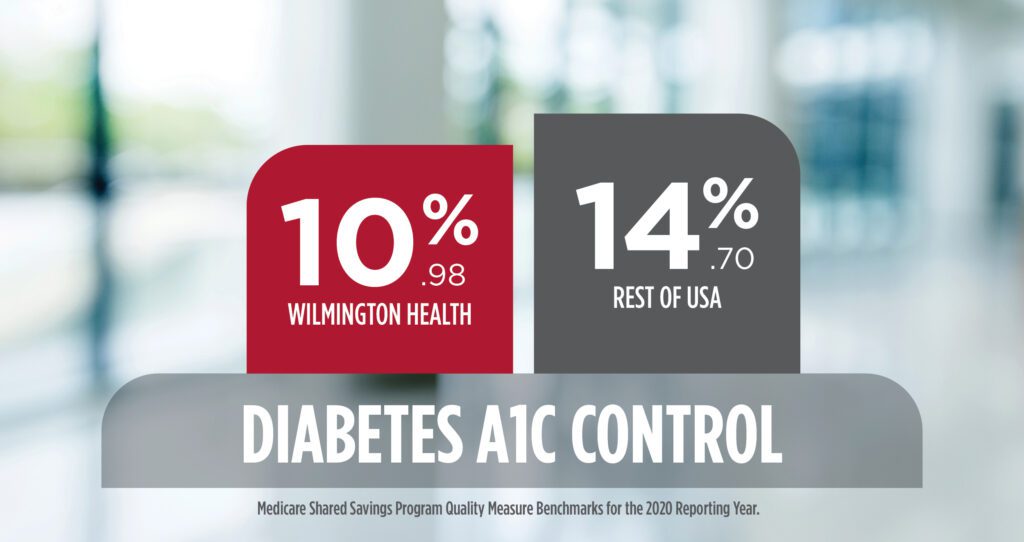
Wilmington Health continues to have a lower percentage of patients with elevated A1C levels than the national average. After a patient is diagnosed and knows their A1C, our team can counsel them on lifestyle changes to lower the number, prescribe medications if needed, and schedule follow-up appointments to monitor the patient. By engaging patients in their health care, we can work together to reach these health goals.
